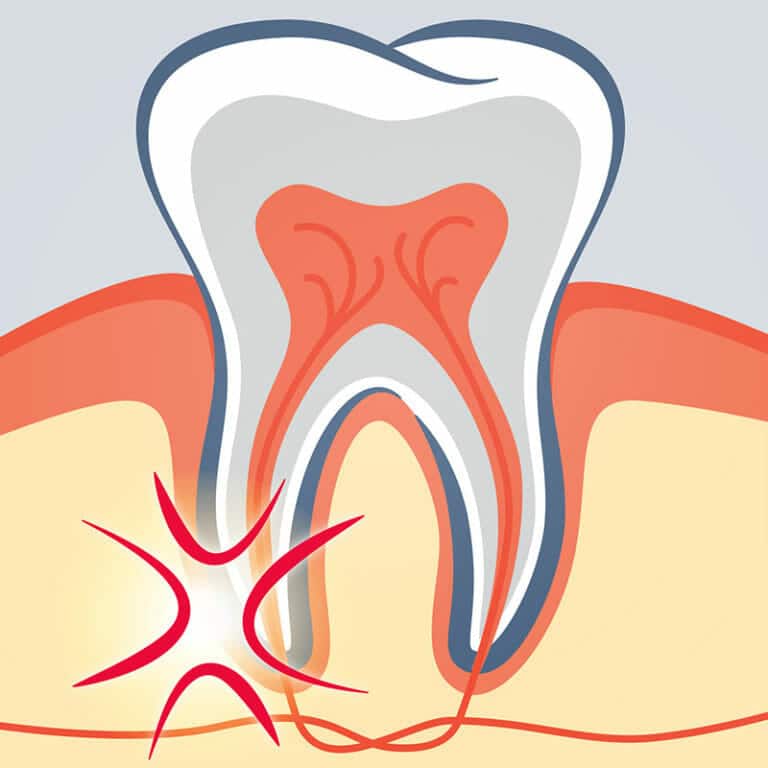
A tooth is composed of several layers. Beneath the outer layer of white enamel that you see in the mirror is a hard layer called dentin. Dentin provides additional support for the enamel as well as the structure of the tooth, but it also protects the soft tissue inside the tooth called the dental pulp. Dental pulp contains nerves, blood vessels, and connective tissue to feed the tooth’s root during growth and development. For this reason, dental pulp is especially important in younger people, but fully developed teeth can survive without it, drawing the nourishment they need from surrounding tissue.
Sometimes, this pulp can become damaged, inflamed, or infected as a result of:
- Injury to the tooth, such as from a blow to the jaw
- Multiple dental procedures to the same tooth
- Extensive decay from an untreated cavity
- A crack or chip in the tooth
- Faulty or damaged crowns
The damaged pulp can begin to deteriorate or decay, allowing bacteria to enter the inside of the tooth and multiply, causing an infection of the pulp or an abscess, a pus-filled pocket at the tip of the tooth’s root.
If left untreated, an infected or abscessed tooth can lead to:
- Bone loss around the end of the root
- A hole in the side of the tooth that allows drainage from the root into the gums or through the cheek
- Swelling in other parts of the face, head, or neck
- Infection that spreads to surrounding gum tissue or bone
- Tooth loss
Once the pulp has become inflamed or infected, the only way to save the tooth is through a root canal. A dentist will perform an examination and an X-ray to confirm this.
What is a root canal treatment?
A root canal, also called endodontic treatment, is a dental procedure that removes the infected or inflamed pulp of a tooth to save the tooth, relieve pain, and prevent reinfection. During the procedure, the inside of the tooth is cleaned and disinfected, then filled with a paste or other synthetic material like gutta-percha and sealed with a crown or filling.
Signs you may need a root canal include:
- Swelling or tenderness in the surrounding gums
- Tooth or gum discoloration
- Sensitivity or pain to hot or cold temperatures, even after exposure
- Severe tooth pain with pressure or chewing
Who performs root canals?
Root canals can be performed by either a dentist or an endodontist, a dental professional who specializes in dental pulp. Depending on the complexity of the case, most dentists will refer patients to root canal specialists. Endodontists have completed additional training beyond dental school, training which includes diagnosing tooth pain, pain management, and other procedures necessary for saving natural teeth. An assessment of your situation, including the severity and extent of the damage, will determine who is best suited to perform your root canal.
What is involved in a root canal?
A root canal treatment is similar to a routine filling, and, depending on the extent and severity of the damage, can often be completed in one or two appointments at a dental office. The dentist or endodontist will apply a numbing medication on the gum surrounding the affected tooth before injecting a local anesthetic, which feels like a quick but sharp pinch or burn. This will prevent any pain during the procedure, during which most patients remain awake.
Once the tooth is numb, the dentist or endodontist will drill a small hole in the top of the tooth to expose the dental pulp. The pulp will be cleaned out and the inside of the tooth coated with an antibiotic to ensure the infection is clear and prevent reinfection. A sealer paste or other synthetic material, like gutta-percha, will be used to fill and seal the tooth, followed by a temporary filling and sealant.
Though you may experience some numbness or discomfort for a few hours after the procedure, most patients return to their normal routines the same day.
A second appointment may be required if the dentist or endodontist recommends a permanent filling or crown for the tooth.
Are root canals common?
Root canals are a common, standard procedure for saving infected teeth, with more than 15 million performed every year in the U.S. This means the average endodontist—a root canal specialist—performs approximately 25 root canals every week!
How effective is a root canal?
As with most dental care, root canals have evolved dramatically over the decades, now boasting a 95% success rate. Properly performed root canal treatments can ensure the repaired tooth lasts a lifetime with little to no additional future dental work required.
How painful is a root canal?
Root canals are performed under local anesthesia and generally no more painful than other routine dental procedures like wisdom teeth removal or fillings. However, as with other dental procedures, there may be some numbness, soreness, or mild discomfort for 24-48 hours after the root canal treatment as a result of tissue inflammation. For most patients, the pain of the infected tooth is significantly greater than any pain or discomfort felt post-procedure.
What are the benefits of a root canal?
Root canal or endodontic treatments are critical for rescuing, repairing, and restoring infected or abscessed teeth. If left untreated, the infected or inflamed dental pulp inside the tooth can ultimately result in wide-spread infection, tooth loss, or even loss of part of the jaw bone. Preserving the natural tooth allows you to retain a natural appearance, normal biting force and sensation, and proper chewing mechanisms. It also helps protect other teeth from excessive wear or strain and reduce the chances you’ll need more restorative dental work in the future.
What are the alternatives to a root canal?
The only way to save a natural tooth with damaged, inflamed, or infected dental pulp is to remove the pulp via a root canal; neither cleanings nor fillings will address the problem. As such, the only alternative to a root canal would be tooth extraction, which is the removal of the entire tooth. To maintain proper oral function—including chewing, speaking, and dental alignment—the tooth would need to be replaced with an implant, bridge, or partial denture. Tooth extractions are a permanent loss of a natural tooth, and no restorative options other than dental implants will feel or function like having a natural tooth. Root canals allow dentists to save teeth, while extractions are a last resort for most dentists and endodontists.
How safe is a root canal procedure?
Root canal treatment is extremely safe and effective, especially when performed by a trained endodontic specialist (a dental professional who specializes in root canals). Root canals have been performed for over 200 years, and advancements in technology, instruments, techniques, disinfectants, and pain management continue to make the treatment even more predictable and successful. Root canals are intended solely to preserve a natural tooth and prevent any reinfection and are much safer than the alternative to an infected tooth—tooth extraction.
What is the best way to recover from a root canal?
Because of the local anesthesia, your mouth will be numb for 2-4 hours following a root canal procedure, though most patients return to work or school the same day. The best way to recover from a root canal is to treat any sensitivity or discomfort with over-the-counter pain medications like naproxen or ibuprofen and to avoid eating anything until the numbness is entirely gone to prevent damaging the newly-repaired tooth without knowing it. Continue with good oral care, including brushing and flossing; attend all follow-up appointments; and keep regular bi-annual cleaning and exam appointments.
What is an emergency root canal?
An emergency root canal is not necessarily much different than a scheduled or planned root canal; both result from the same cause—inflamed or infected dental pulp inside a tooth. However, the treatment has probably become an emergency because the inflammation or infection has gone untreated too long and the pain is now unbearable, the tooth is severely damaged, or there is pus oozing from around the tooth. If you are experiencing any of the symptoms of an infected tooth (swelling or tenderness in the gums, tooth or gum discoloration, extreme sensitivity, or severe pain when chewing), your best option is to contact a dentist right away and avoid the emergency altogether.
To learn more about root canal services at Dental Depot, contact a Dental Depot nearest you to reserve an appointment.